Annual Report 2017 - 2018
Message from the President, 2017 – 2018
Scot B. Glasberg, MD
Message from the President, 2017 – 2018
Scot B. Glasberg, MD



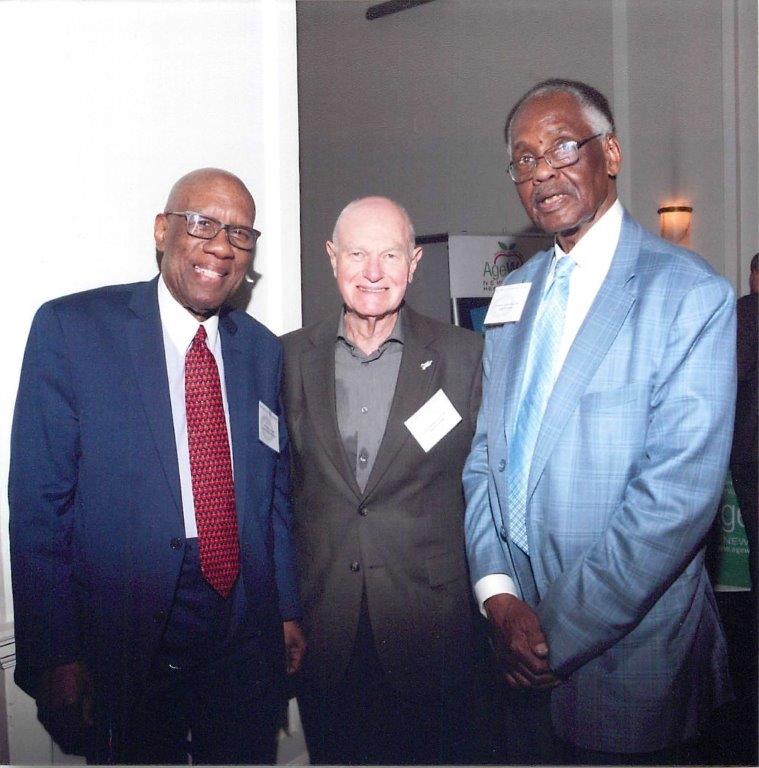
Photo 1:Incoming President Naheed Van de Walle, MD, with President Scot B. Glasberg, MD, at the New York County Medical Society’s 2018 Annual Meeting, June 20, 2018. Photo by Mervyn Bamby
Photo 2: June 20, 2018, Annual Meeting of the New York County Medical Society: Paul N. Orloff, MD accepts the Nicholas Romayne MD Award from President Scot B. Glasberg, MD Photo by Mervyn Bamby
Photo 3: June 20, 2018, Annual Meeting of the New York County Medical Society: Thomas J. Madejski, MD, President, Medical Society of the State of New York, presents President Scot B. Glasberg, MD with a commendation from Governor Mario Cuomo Photo by Mervyn Bamby
Photo 4: June 20, 2018, Annual Meeting of the New York County Medical Society: Past presidents Milton Haynes, Kenneth Brookler, and Anthony Clemendor catch up. Photo by Mervyn Bamby
The last official duty for each president of the New York County Medical Society is the President’s Message in the Annual Report. It is an honor to be part of this tradition and continue the lineage of the Medical Society presidents.
I am pleased to report to you that during the past year our focus has been working on solutions, not just listing our troubles when it comes to legislative activities. My mantra during my term has been that we cannot be the party of “No.” We must be willing to negotiate with those with whom we disagree in order to see results.
One example has been our continuing discussions with Assemblymember Richard Gottfried and Senator Gustavo Rivera on single payer legislation. We need to be realistic about politics in New York State even as we contrast our support for universal healthcare as opposed to single payer. Our discussions with legislators have been designed to ensure fairness for physicians IF single payer legislation is passed (especially after the turnaround in New York State Legislature last fall). Rather than focusing only on what we don’t like, we are negotiating for what would be good for physicians, such as elimination of pre–authorization requirements and opportunities for collective negotiation. At the same time, we are talking about the realistic questions that have to be answered with any complex change in health care.
In addition to advocacy efforts, we continue to work on behalf of our members — we brought more benefits to the table, including an introduction to a new medical liability insurance company. We worked for cleaner communications and more programs. We amended our Bylaws and brought in new leadership on the Board. We relocated to new space to keep costs down.
The leadership of the past year is listed in this report. I am grateful for the support and hard work of this group, and you should be as well. We have looked at a number of issues from how to be effective at gaining our political goals to maneuvering the various approaches different specialties take to maintenance of certification. No matter the question, I found my fellow Board members to be all the things good Board members should be — thoughtful, provocative, skeptical, proactive, caring, and cognizant of their duty to the organization and to you, the members.
On behalf of all of us, thank you for the opportunity to represent our profession and this Society in its 112th year of operation.
Elected in 2018
| Active | 4 |
| Young Physician/Part Time Paid Retired | 49 |
| Resident/Fellow |
47 |
| TOTAL | 100 |
CURRENT MEMBERS IN 2018
| Active | 800 |
| Associate | 0 |
| Student | 678 |
| Life | 762 |
| Reduced Rate | 291 |
| TOTAL | 2,621 |
Figures reflect membership as of 12/31/2018
In accord with Article VI, Section 6 of the Bylaws of the New York County Medical Society, I present this statement summarizing the Society’s financial records for the fiscal year ending June 30, 2018. Any active member in good standing may, by appointment, inspect the full and complete statement of our independent accountants at the offices of the Society.
Jill Baron, MD, Treasurer
| Income | |
| Dues and Commission | $407,431 |
| Grants and Contributions | 75 |
| Fees | 86,425 |
| Royalties and Adminstrative Fees | 76,848 |
| Reimbursments | 3,638 |
| Advertising | 17,457 |
| Other income | 6,388 |
| Total Income | $ 598,262 |
| Expenses | |
| Salaries and Related Expenses | $309,998 |
| Occupancy Costs | 91,763 |
| Business Expense | 1,536 |
| Program Activities and Functions | 55,033 |
| Office Managment | 57,385 |
| Professional Services | 62,721 |
| Total Expenses | $578,436 |
| INCOME OVER EXPENSES | $19,826 |

Photo 1: The Presidents, June 20, 2018, Annual Meeting of the New York County Medical Society: Back row, left to right: Kenneth H. Brookler, MD; William B. Rosenblatt, MD; Joshua M. Cohen, MD, MPH; Andrew T. Cheng, MD; Malcolm D. Reid, MD, MPP; Peter C. Lombardo, MD; and Milton Haynes, MD; Front row, left to right: Zebulon Taintor, MD; Michael T. Goldstein, MD, JD; Paul N. Orloff, MD;; Scot B. Glasberg, MD; and Naheed Van de Walle, MD Photo by Mervyn Bamby
Board of Directors,
New York County Medical Society
Scot B. Glasberg, MD, President
Naheed Van de Walle, MD, President–Elect
Mimi Buchness, MD, Vice President
Jessica J. Krant, MD, MPH, Secretary
Arthur Cooper, MD, Assistant Secretary
Ami Shah, MD, Treasurer
Jill Baron, MD, Assistant Treasurer
Board of Medical Ethics
Ksenija Belsley, MD
Michael Borecky, MD
Erick Eiting, MD
Milton Haynes, MD
Steve Young Lee, MD
Henry Magliato, MD
Marlin Mattson, MD
Board Members at Large
Loren Wissner Greene, MD
Keyvan Jahanbakhsh, MD
Keith LaScalea, MD
Patricia McLaughlin, MD
Mark Milstein, MD
Bijan Safai, MD
Gabrielle L. Shapiro, MD
Robert Sporter, MD
Thomas Sterry, MD
MSSNY ex–officio
Joshua M. Cohen, MD, MPH, Councilor
Malcolm D. Reid, MD, MPP, MSSNY Past President
Board of Trustees, New York County Medical Society
Board of Directors, Spingarn Fund, Inc.
Peter C. Lombardo, MD, Chair
Paul N. Orloff, MD
Joshua M. Cohen, MD, MPH
Edward W. Powers, III, MD
Michael T. Goldstein, MD, JD
Committee Chairs,
New York County Medical Society 2017 –2018
Naheed Van de Walle, MD, Continuing Medical Education
Peter Lombardo, MD, Public Health
Heskel M. Haddad, MD, Parking Review
Milton Haynes, MD, Bylaws
Keyvan Jahanbakhsh, MD, Young Physicians
Paul N. Orloff, MD, Government Affairs
Scot B. Glasberg, MD, Membership Benefits
Steven Zaretsky, MD, Workers’ Compensation
Michelle Zweifler, MD, Public Relations
Delegation to the Medical Society
of the State of New York Leadership
William B. Rosenblatt, MD, Chair
Anthony A. Clemendor, MD, Vice Chair
Stuart Orsher, MD, JD, Chair Emeritus
Scot B. Glasberg, MD, Presidential Vice Chair
Robert B. Goldberg, DO, AMA Delegate
Malcolm D. Reid, MD, MPP, MSSNY Past President and AMA Delegate
Joshua M. Cohen, MD, MPH, MSSNY Councilor, AMA Alternate Delegate
Staff, New York County Medical Society
Cheryl M. Malone, CAE, Executive Director
Susan Tucker, Esq.
Sony Hilado
Lisa Joseph
March 2019 Issue
Physician Advocacy Day A Success
Free Dinner Program and Crucial CME April 18
Letter from a Member to a Legislator
Urge Legislature to Oppose Cuts to Payments for Medicaid/ Medicare Dual–Eligibles
“Train the Trainers” Sexual Harassment Webinar:
NGS Medicare Releases Educational Chart Outlining 2019 E/M Changes
Patient Feedback Survey: How Asking the Right Questions Can Help Your Practice
Performing a Security Risk Assessment Offers Value Beyond Compliance
Protect Your Document Security
New York Maternal Mortality Spikes, Part of Nationwide Issue
Updated Workers’ Comp Schedule Auto No–Fault Delayed
CMS Issues Quality Payment Program: 2019 Resources
Free CME Program on Adolescent Sexual Health
Dues Deductions for 2018 Taxes
How Can You Save When You Bill?
Tips for Medical Practice Recruiting Success
Comment Period Open for Xcertia (Digital Health Apps Guideline)
Don't Throw Your Money Away with the Waste
US Air Force Programs Available for Physicians and Students
This feature of MM “NEWS” introduces you to Society leaders as they explain their vision of organized medicine’s activities. This month, read Society President Naheed Van de Walle’s message (picture below).

Physicians as Advocates
Dear Colleagues,
Having just returned from a full day of lobbying for the multitude of health care issue that have transformed the practice of medicine, it would be appropriate to look deeper into what Physician Advocacy really is.
Our role as advocates is not new and goes back since the inception of the profession. We have been advocating for our patients intuitively whenever our patients cannot access the care they deserve. This is deeply ingrained in our psyche. We know what effect denial of health care services has on our patients on a daily basis. We spend inordinate amount of our time fighting for our patients’ right to have access to basic care.
Since the advent of ‘Managed Care,” as entities routinely ration healthcare and physician reimbursement, it has become imperative for us to advocate for our patients and the dedicated physicians who have devoted their lives to delivering the best possible care to their patients. Over the past couple of decades changes in the healthcare system have been significant and sweeping, which in many cases have been detrimental for the patients and have tied the hands of physicians who deliver the care.
Physician reimbursement has been a major target when decisions about cuts in healthcare spending are made. Out of the 3.9 trillion in healthcare spending, only 15 percent goes towards physicians. Administrative costs have skyrocketed as reimbursements drop. In a hospital setting, for every 10 physicians, there are seven staff members engaged in billing. In addition to that work, physicians spend several hours each day dealing with paper work. According to one estimate, physicians spend 27 percent of their time interacting with their patients and 49.2 percent of their time on completing medical records and other paperwork.
There is obviously something very wrong with this type of healthcare model. It leads to fragmentation of the patient/physician relationship and patient dissatisfaction, among other issues.
How Do Lobbying and Advocacy Differ?
The American Medical Association endorses a commitment that states that physicians must “advocate for social, economic, educational, and political changes that ameliorate suffering and contribute to human well–being”
Advocacy is generally defined as arguing in favor of a cause or idea, whether its environmental protection, minority rights, or the myriad other issues that affect people every day. There is no limit to the amount of advocacy a person or organization (such as a nonprofit) can do.
Lobbying can generally be defined as any attempt to influence a politician or public official on an issue. Lobbying is further broken down into:
Direct lobbying: Any attempt to influence new or existing legislation via communication with a member of the legislative body or other government representative who has a say in the legislation.
Grassroots lobbying: Asking the general public to contact their legislator and/or mobilizing the public around a legislative issue. Examples of grassroots lobbying include creating an online petition to generate public support for a cause, distributing flyers, and organizing a public demonstration or rally.
Physicians can advocate at various levels. At an individual level for the patient, at a regional level to effect changes in a community or at a system level to promote strategies that improve the impact of healthcare changes overall.
If advocacy is so important for physicians and practice medicine, then why is it that more physicians do not actively participate in advocacy. There are several reasons for that. There is some degree of ambiguity about the role of physicians as advocates, and poor definition of boundaries and scope of advocacy. Although most physicians believe in the concept of advocacy, they do not actively participate in the process due to lack of time, lack of requisite skills, and lack of clarity about their roles as advocates, as noted by Mark A. Ernest, MD in his article “Physician Advocacy: What Is It and How Do We Do It?” published in Academic Medicine, vol. 85, no. 1– January 2010. He states “Despite widespread acceptance of a physician’s duty to advocate, the concept remains problematic because it remains undefined.”
Thomas Huddle, MD, who authored the article “Medical Professionalism and Medical Education Should Not Involve Commitments to Political Advocacy,” published in Academic Medicine: March2011–Vol.86–issue 3–pp. 378–383 gives a different perspective. Doctor Huddle believes that political advocacy, if it is a virtue, is a civic virtue rather than a professional one. This point of view does not hold true for many others who are proponents of physicians as advocates.
If we are to consider physician advocacy as our professional imperative, then we have to take steps to educate physicians from very early on to acquire the skills needed to advocate for the patients and the profession. Such a process has to be done in a thoughtful and deliberate fashion by fostering changes at the undergraduate and graduate level. It represents a big shift from the current paradigm where undergraduate and graduate medical education has focused purely on developing clinical competence. It would also require mentors who could pass these skills on to their mentees. These changes are quite complex and require support of Liaison Committee on Medical Education and ACGME as well as many other changes.
Currently, advocacy is carried out largely through State, Specialty, and National Medical Societies providing opportunities to physicians new to the process to learn the skills from more experienced physicians. Ongoing healthcare changes affect the lives of all physicians and our patients. We therefore need increased physician participation in advocacy efforts.
If we are to make the lives and health of our patients and physicians better, then we ought to continue the efforts to train and educate our peers to do the same because the Status Quo is not sustainable.
I will end here with a quote by someone wiser than myself:
“Never doubt that a small group of thoughtful, committed citizens can change the world. Indeed, it is the only thing that ever has.”
-Margaret Mead
Physician Advocacy Day A Success
If you “lobbied from your desk” on March 6, 2019, during MSSNY’s Annual Physician Advocacy Day, THANK YOU! We appreciate your reaching out to advocate for the profession and your patients.
However, we ALL owe special thanks to these New York County doctors who joined us on legislative visits to 15 Manhattan assemblymembers and senators. It’s a busy day (but the camaraderie is excellent). The most impressive part is watching a group of doctors of all specialties and stages of practice sharing their stories, statistics, and points with legislative offices.
Thanks to these physician leaders for a great day representing all our members AND patients.
Naheed Van de Walle, MD, President
Arthur Cooper, MD, Vice President
Paul N. Orloff, MD, Chair, Board of Trustees, Chair, Government Affairs
Edward W. Powers, III, MD, Board of Trustees
Michael Borecky, MD, Board of Directors
Gabrielle Shapiro, MD, Board of Directors
Malcolm D. Reid, MD, MPP, Trustee, MSSNY
Antigone Argyriou, MD
Moshe Bressler
David Bronheim, MD
Christopher Clifford, MD
Jennifer Cushman
Connie Di Mari, MD
Richard Ellis, MD
Samantha Erosa, MD
Jacob Levitt, MD
Lawrence Melniker, MD (Kings County)
Jeanne Rosenthal, MD
Rishi Kamlesh Thaker, MD
Parda Valluru, MD
Robert Wu, MD
Free Dinner Program and Crucial CME April 18
Register today for a great FREE CME program presented by the New York County Medical Society and The Doctors Company. Join us on Thursday, April 18, 2019,
5:30 p.m. Registration, 6:00 p.m. to 8:30 p.m., at the Midpoint Bistro, 40 West 45 Street (between Fifth and Sixth) for 2.5 Category I CME credits and a light supper as we present:
“Personal Electronic Device Distraction and the Threat to Patient Safety”
“Electronic Health Record: Ten Years and Still Risky”
There is no charge, but space IS limited so pre–registration is required! Register with Lisa Joseph at This email address is being protected from spambots. You need JavaScript enabled to view it. or (212) 684–4698.
We thank The Doctors Company, the Society’s endorsed medical liability company, for providing this program with speakers Lisa M. McCorkle, Senior Patient Safety Risk Manager, Department of Patient Safety and Risk Management, NE Region, The Doctors Company, and Maureen M. Arciero, Esq., Schiavetti, Corgan, DiEdwards, Weinberg & Nicholson, LLP.
“Personal Electronic Device Distraction and the Threat to Patient Safety”
Healthcare delivery, when distracted by electronic devices, can potentially lead to unsafe care. Self–imposed use of such devices for non–medical purposes has seeped into daily practice. Personal electronic devices can create a digital distraction so engaging that it consumes situational awareness, potentially preventing healthcare providers from focusing on, caring for, and interacting with patients. Physician/patient interaction with electronic devices brings risk as well. Patients can use their own technology to record physician interactions, sometimes surreptitiously. This program explores the problems of distractions in healthcare practice, and other challenges presented by electronic devices. Case examples with legal counsel reflection and mitigation strategies that can be implemented in your practice will be presented.
Objectives:
- Assess my practice/organization for opportunities to limit distractions and interruptions.
- Identify mitigation strategies to address patient–initiated healthcare recording and other risks associated with electronic devices.
- Create a written plan for my practice that outlines steps to reduce distractions from electronic devices when caring for patients.
- Educate colleagues to the challenges of defending medical malpractice claims involving allegations of distracted practice.
“Electronic Health Record: Ten Years and Still Risky”
It has been ten years since the HITECH Act stimulated the adoption of the electronic health record (EHR) in the United States. With the transformation of nearly all hospitals and ambulatory practices to an EHR, there have been many improvements in the delivery of care. The EHR has also brought the potential of liability exposure for physicians and other care providers. A discussion will be part of this activity looking at the increasing growth and use of medical scribes and their role working with the EHR. A recent ten year EHR–related closed claims study will shed light on risks that have occurred and can still occur including case examples. Risk mitigation strategies will be identified to support practice change and enhance the delivery of safe and quality care for patients.
Objectives:
- Assess the two categories of contributing factors to EHR–related claims.
- Self–reflect on my use of copy and paste, workarounds, alert fatigue and other potential dangers of the E H R and implement one practice improvement measure.
- Seek out EHR training as needed to enhance self–learning and optimize EHR use.
- Evaluate the risks of using scribes in EHR documentation.
Register today with Lisa Joseph at This email address is being protected from spambots. You need JavaScript enabled to view it. or (212) 684–4682.
These nominees were selected by the Society’s Nominating Committee at its meeting on February 18, 2019.
Arthur Cooper, MD, President–Elect
Keith La Scalea, MD, Vice President
Jessica J. Krant, MD, MPH, Secretary
Thomas Sterry, MD, Assistant Secretary
Jill Baron, MD, Treasurer
Erick Eiting, MD, Assistant Treasurer
Naheed Van de Walle, MD, Trustee
Board Members At Large
Ksenija Belsley, MD
Michael Borecky, MD
Stuart Gitlow, MD
Loren Wissner Greene, MD
Keyvan Jahanbakhsh, MD
Mark Milstein, MD
Linda Nicoll, MD
Ami Shah, MD
Gabrielle Shapiro, MD
Delegates to the Medical Society of the State of New York (MSSNY)
Mimi Buchness, MD
Arthur Cooper, MD
Stuart Gitlow, MD
Paul Orloff, MD
Naheed Van de Walle, MD
Alternate Delegates to MSSNY
Ksenija Belsley, MD
Dennis Gage, MD
Michael Borecky, MD
Loren Wissner Greene, MD
Heskel M. Haddad, MD
Keith LaScalea, MD
Thomas Sterry, MD
Letter from a Member to a Legislator
The following letter from Society member Connie DiMari, MD, was sent to Assemblymember Richard Gottfried following the Society’s Legislative Breakfast on January 27. We appreciate Mr. Gottfried’s attendance at the event, and we especially thank Doctor DiMari for coming, asking questions, and taking the time to write this thoughtful response to him following.
Thank you for attending the breakfast and responding to our questions. In your initial statement, you praised hospitals staffed by employed physicians and questioned why physicians wanted to be in private practice (and have to pay the phone bills).
My father had just been discharged from a hospital, and I mentioned my frustrations with competent physicians forced into a constant daily rotation resulting in a lack of continuity of care, critical thinking, and collaboration.
I encountered hospitalists making hasty decisions, anxious to either get my father into an OR, or procedure room, or out of the hospital. Physicians were organized in a way to maximize profits for the hospital and their large group practices — but not in a way that best served patients.
You responded that this was a problem for the profession to solve. I strongly disagree. The Affordable Care Act, in making independent practice very difficult, put control of most physicians firmly in the hands of large group practices and hospitals and their work structured to maximize their employer's bottom line. It is not unusual to see physicians pushed to see 35 – 40 patients a day on an inpatient or outpatient basis. We are schooled on "team"–based care with the goal of seeing an ever–increasing number of patients. We now are pushed to relegate documentation, patient instructions, and even electronic orders to medical assistants with little training.
Sadly, the days are long gone when your primary care physician — who knew you best — was the coordinator of your care and acted as your advocate. That individual was the physician charged with gathering information from consultants, weighing the risks, and helping the patient to make the best decisions. It was always clear from the hospital chart who bore responsibility for the patient. In my father's case, I felt that I was that physician. It was an uncomfortable role for an ophthalmologist, but as a physician with decades of experience, I was able to ask the right questions, insist that alternatives be considered, and information communicated. This would be almost impossible for someone without a degree in medicine.
Having a constant rotation of hospitalists managing care is like having a constant rotation of journalists writing one story, architects and engineers involved in a building design, classroom teachers or lawyers presenting a case. How cogent would that article be without a lead writer or editor giving the story one voice? How well would the building get built without a project manager to resolve design issues? How well could children learn? How could a good defense emerge if the lawyers involved changed every few days without knowing what their predecessors had presented? In all of these cases, someone — whether a lead writer, a project manager, teacher or lawyer — is always there throughout the process, in charge of listening to the different voices, and managing the effort. Physicians are not supermen and superwomen who can drop into situations and know exactly what to do, receiving a brief verbal sign–off and reams of data in an electronic record. For my father the choices were not easy. Choosing between risking a pulmonary embolus, versus a potentially dangerous procedure to prevent an embolus, versus the possibility of a massive hemorrhage — all of which are potentially life-threatening — is not an easy calculation for a 90–year old who just wanted to get home to play bridge. Hopefully I managed to draw out the middle path, and thus far he is, thankfully, doing well.
My opinions have been shaped by my experiences at St. Vincent's Hospital, where I arrived in 1981 to train, and where I subsequently practiced ophthalmology until the hospital shut its doors. At that time all physicians were in private solo or small–group practices. They were able to focus on what was in the best interests of the patient. Critical thinking and debate were encouraged. Erring on the side of the patient in all decisions was the bottom line to be prized.
Now insurance companies and government mandates have deftly managed to create conflicts of interests between doctors and patients. A Harvard–trained mammographer told me she now had to be concerned about calling too many patients with questionable findings back for extra films, as the insurance companies would reimburse her hospital less. How long would her hospital continue to employ a careful physician, if income kept dropping? Predictably, it has now been shown that ACA's mandated decrease in hospital reimbursement — punishing high readmission rates — has resulted in higher death rates. Not surprisingly, this has been particularly damaging to inner city hospitals, which serve the poor.
I believe there is a mistaken assumption that an employed physician has little incentive to over treat. This is very wrong. I believe that the decision making of hospitalists, with their employer in mind, becomes more reflexive, less considered, naturally more aggressive, and less conservative, even when dealing with a 90–year-old.
I have seen physicians pushed out of practices and hospital associations if they did not generate the income expected. I read statistics concerning the money generated by procedures performed by various specialists for the hospitals where they work: a gastroenterologist generates $1.5 million, a cardiologist $1.8 million, a neurosurgeon $2.5 million. With numbers this big, I can't believe hospitals aren't watching each physician's generated dollars very closely. The jobs of these physicians are on the line.
Sincerely,
Connie DiMari, MD
Urge Legislature to Oppose Cuts to Payments for Medicaid/ Medicare Dual–Eligibles
All physicians are urged to contact their State legislators to urge that they reject a proposal contained in the 2019 – 2020 Executive Budget that would significantly cut the payments that Medicaid makes to physicians to cover the Medicare Part B deductibles of their “dually eligible” patients.
This proposal would reduce payments to cover Medicare Part B deductibles to the Medicaid rate, cutting physician payment by 44 percent for these services. Representatives need to understand the dire impact that this will have on practices, and thus on the patients that you treat.
Send a letter to your State Legislator by clicking the link here.
https://cqrcengage.com/mssny/app/write-a-letter?0&engagementId=495714
“Train the Trainers” Sexual Harassment Webinar:
New York State recently mandated that all employers are required to have a sexual harassment policy containing specified criteria in place by October 9, 2018, and to conduct sexual harassment prevention training by October 2019. (New York City requirements are slated to take effect in April 2019.)
The Medical Society of the State of New York General Counsel Garfunkel Wild will be offering a complimentary webinar “Train the Trainers: The Impact on the Healthcare” on March 20, 2019, 12:00 p.m. – 1:00 p.m. MSSNY also will be placing a recorded version on its website
Register at https://register.gotowebinar.com/register/3781044962772504323
The following is courtesy of James McNally, the Society’s Third–Party Insurance Help Program. If you have questions, call the Society at (212) 684–4681.
- REMINDER: eMedNY Physician Anesthesia, Drug, Medicine, Radiology, Surgery and Vision Care Fee Schedules Updated: The Physician Anesthesia, Drug, Medicine, Radiology and Surgery Fee Schedules have been updated. For more information, click on the link here.
https://www.emedny.org/ProviderManuals/Physician/index.aspx
In addition, the Vision Care Fee Schedule has also been updated at the link here.
https://www.emedny.org/ProviderManuals/VisionCare/index.aspx
- NY Workers Compensation Board to Increase Fees Effective April 1, 2019:
The New York Workers Compensation Board (NYSWCB) will initiate an overall 5 percent increase in the medical fee schedule for care to injured workers effective April 1, 2019.
The WCB will increase the physician deposition and hearing testimony fee from $400 to $450 effective April 1 as well. Payment of these fees shall be paid by the carrier within ten days of the testimony. Physicians who have not been paid within that time frame should contact the WCB for enforcement.
- Attention: EIDM Users – You May Need to Create an Account in HARP to Access Your QPP MIPS Data: On December 19, 2018, CMS transitioned to a new system to create identity management accounts and to request access to the Quality Payment Program (QPP) website called The Healthcare Quality Information System (HCQIS) Access Roles and Profile (HARP) system. If you previously created a QPP account in the Enterprise Identity Management (EIDM) system, continue to use your EIDM ID and password to sign-in, view, submit, and manage your data. If you need to make any changes to your ID/password or create a new account, you will now do so in the HARP system.
You can view videos for step-by-step instructions on how to:
- Connect to an Organization: Practice — View, submit, and manage data on behalf of the practice: https://www.youtube.com/watch?v=3zS03Jmas1U
- Create a QPP Account — Create a new HARP account: https://www.youtube.com/watch?v=4xGkWvPa33E&feature=youtu.be
- Connect to an Organization: APM Entity — View, submit, and manage data on behalf of the APM: https://www.youtube.com/watch?v=3NVv9VKomOk
- Connect to an Organization: Registry — Submit data on behalf of your customers: https://www.youtube.com/watch?v=c0Tp61xSBDY
- Connect to an Organization: Virtual Group — View, submit, and manage data on behalf of the virtual group: https://www.youtube.com/watch?v=SvBZgdo_TVg
- Security Officials: Approving Role Requests — Approve and deny requests from staff users: https://www.youtube.com/watch?v=Fy3fnkZZClI&feature=youtu.be
For more information, contact This email address is being protected from spambots. You need JavaScript enabled to view it. or call (866) 288–8292.
CMS To Issue Corrections to 2019 MIPS Payment Adjustments Related to Part B Drugs:
Recently, CMS discovered an error in the implementation of the 2019 Merit–based Incentive Payment System (MIPS) payment adjustment; it incorrectly applies payments for Medicare Part B drugs and other non–physician services billed by physicians. Adjustments to impacted claims will occur soon:
- If they overpaid a claim based on this error, you will get a notification for recoupment from your Medicare Administrative Contractor.
- If they underpaid a claim, it will be adjusted.
You do not need to do anything.
Physicians and Non–Physician Practitioners — New Medicare Enrollment Application: CMS received approval for a new Medicare Enrollment Application for physicians and non-physician practitioners (CMS-855I dated 12/2018). Many changes are minor; the major ones reduce provider burden:
- eliminated reporting for advanced diagnostic imaging, Clinical Laboratory Improvement Amendments number, and the Food and Drug Administration radiology certification number;
- expanded instructions for individual and group affiliations to simplify reporting;
- made it optional to list a contact person;
- added electronic storage information for those who no longer keep paper records; and
- created a more logical data flow.
You may begin using the new application immediately. Through April 30, Medicare Administrative Contractors will accept applications dated 7/2011, but after that, you must use the new version.
If you have questions on any of these issues, contact the Society’s Third–Party Insurance Help Program at (212) 684–4681.
NGS Medicare Releases Educational Chart Outlining 2019 E/M Changes
NGS Medicare has posted an educational chart outlining the 2019 changes to the Evaluation & Management code documentation requirements. It also shows the policy points related to the new Interprofessional Consultation codes.
To review this chart, go to the link here:
What’s Changed as a Result of CMS Final Rule 2019
Patient Feedback Survey: How Asking the Right Questions Can Help Your Practice
The following article is supplied by Alex Mangrolia from Practice Builders.
If you want to download. Practice Builder’s check list to make sure your practice website is on the first page of google, go to https://www.practicebuilders.com/first-page-ranking1/?utm_source=NYCMS
A nicely crafted patient satisfaction survey is one of the best methods practices have for understanding their strengths and knowing what they should improve.
Surveys are an excellent way to assess patient satisfaction, brand potential, service quality, price comparison and much more. However, there are right and wrong ways to frame survey questions. The way you write your survey questions has a direct impact on the response rate as well as the efficacy of the responses.
Getting Started With Surveys
Simply put, patient surveys help you find answers to different business questions. Of course, the better the quality questions you ask, the better responses you will get. And, in the context of conversion optimization, asking inappropriate questions can lead you down the wrong path.
Therefore, for your patient experience and conversion research efforts, it is important to spend a little more time on creating meaningful questions.
As David F. Harris suggested, “If we make survey questions clear, answerable and unbiased, we can reduce the survey length, enhance respondents’ experience and significantly improve the quality of data.”
The right questions are not just about getting you better responses for better decisions. The surveys and the responses can affect your practice’s reputation. Your survey length and questions will either enhance your brand or turn respondents away.
Most practices use online survey tools rather than someone calling patients to ask questions. Online surveys are less pushy than personal calls or questions, and they are easy to put together. Online tools such as SurveyMonkey can help you get an online survey up and running in a matter of minutes.
Even though you can publish your patient satisfaction survey quickly, it is always better to take your time and create effective and thoughtful questions that will generate valuable responses to your medical practice. The right questions can make a big impact on your practice.
Types of Survey Questions
One of the most powerful factors in designing a successful survey is the quality and relevance of your questions. At the end of the day, well–drafted questions are key to every successful survey, whereas poorly structured questions can result in incorrect responses, which are, ultimately, a waste of time.
Thoughtfully crafted questions driven by a strong collection mechanism are imperative in ensuring valuable data. Yet, the importance of using the right question types is often ignored. It is essential to align your question types with the overall framework of your survey.
Make sure you define your survey’s goals, sample size, target audience and survey method before creating the questions. Paying attention to these details can transform the way your target audience will interact with the survey. In addition, you can expect rich dividends in gathering useful data that justifies the purpose of the campaign.
The types of questions you include in your survey can have a powerful influence on the input you are able to gather, and they could be the difference between a survey that helps you make an informed decision and the one that leaves you with more confusion.
Essentially, there are two types of questions you can ask in a survey: open–ended and closed–ended questions.
Open–ended questions require your target audience to answer the questions in their own words. For instance, you might ask, “What did you like the most about your visit today?” Or, “You have used some of our additional services in the past, so why are you no longer using them?”
Open–ended questions can provide you with the most detailed feedback from your patients. You must allow the respondents to give you an honest opinion about your services in their own words. This type of questions will generate useful feedback. However, try not to overuse them. One open–ended question per survey should be sufficient.
Open–ended questions give your patients the opportunity to:
— Use their own words to respond to your questions.
— Show the depth and strength of their thoughts.
— Narrate their experiences as much as they want.
— Give exact representations of personal views.
However, there are some challenges to open–ended questions:
— Answers may vary in length and quality.
— Uninterested patients may not take the time to give you detailed feedback.
— Assessing data can be a tedious and time–consuming process. In addition, you may risk losing some of the rich details that comments can provide.
To sum it up: You may consider using open–ended questions when you are looking for detailed feedback. Open–ended questions may result in some great follow–up questions for gaining additional insights.
Closed–ended questions require your patients to choose from a list of responses that you provide.
For instance, a small practice curious about patient satisfaction may ask, “How satisfied are you with our services?” and provide four response options: Very Satisfied, Satisfied, Dissatisfied and Very Dissatisfied.
Closed–ended questions give your patients the opportunity to:
— Quickly answer the questions since response options are available.
— Responses are easier to compare and analyze.
— In addition, closed-ended questions are faster to summarize. You can easily assess what percentage of your patients selected each answer choice, or you can make a comparison between how two groups of patients answered a question.
Here are some of the limitations of closed–ended questions:
— Uninterested patients may select a random response option, thus decreasing the survey’s credibility.
— Patients may feel frustrated due to the limited choice of response options.
To sum it up: You may consider using closed–ended questions when you have a good understanding of patient behavior and can come up with the correct set of response options for the questions. In some cases, including an “Other” category will help reduce any frustrations your patients feel when they are asked to select from a limited number of response options.
Deciding when to use an open–ended or a closed–ended question is an integral part of survey design. If you look at the opportunities and challenges of each question type, you will be on your way to collecting relevant data that your practice can use to drive decision–making.
Useful Tips
If done well, a patient satisfaction survey that follows best practices can provide eye–opening information — the kind that changes the direction of a medical practice for the better. On the other hand, a poorly drafted survey will yield inadequate data while making the respondent frustrated.
So why do these directionless, agonizing patient surveys persist?
Too often, healthcare marketers fall into the trap of focusing exclusively on their own desire for information, and not on the experience that they create for patients. When this occurs, respondents take a shortcut through the survey, and neither party wins.
In order to correct such errors, we have put together four helpful tips that can push your respondents through the whole survey in a way that creates a positive experience, without compromising on the actionable information.
1. Keep it Simple and Concise
Regardless of your target audience, use simple and straightforward language and tone in all of your questions. Most respondents will not take the time to read a question more than once.
When it comes to patient satisfaction surveys, simplicity is key. This is because you are trying to reach out to people who probably are busy. So it is best to make your questions easy for them to understand and then answer them as quickly as possible. Asking complex questions may confuse respondents. When this happens, two things are bound to follow: Either the respondents will reject your survey or they will give you hasty and incorrect responses.
Brevity is also important. A lengthy survey may cause an incredibly high rejection rate. You want respondents to honestly respond to your questions, and a 50–minute survey cannot support that.
2. Speak Your Target Audience’s Language
When creating a survey, there is often a temptation among healthcare marketers to make the phrasing of questions as bland as possible. This is because a lot of marketers fear that inserting unnecessary content may dilute the results of the survey. This is a valid concern. After all, surveys are not supposed to entertain; they are supposed to extract meaningful information. However, surveys should not be boring. In fact, surveys should engage the participants enough to inspire creative and constructive feedback that can be used to grow and market your practice. Though it is obvious, the best way to write an easy survey is to speak the language of your respondents. This means minimizing the use of words or phrases that may confuse your target users.
3. Limit the Number of Response Options
When you ask your survey participants to rank your services in order of preference or importance, try not to give too many options. While it is difficult to fix the exact number of response options that you can provide, a good tip is to offer a complete list of the most likely choices and then provide an “other” option to collect input from the rest of the responses. Asking your respondents to rate or rank a long list can result in a rejected survey. If you need to get respondents’ feedback on all of the items on your list, consider splitting the original question into two separate questions.
4. Include Open–Ended Questions
Open–ended questions are viewed as risky as they are difficult to quantify. However, open–ended questions can be of great use, and it is important to include at least one or two such questions in your survey. Patients often have a lot on their mind, and allowing them to answer a question in detail can provide you with extensive feedback that you may not have received otherwise.
When asking open–ended questions, you must be careful as some respondents may provide you with long, unnecessary responses. In order to prevent such incidents, provide a text box where target users can write their answers and limit the number of characters the text box can accept.
Conclusion
Once you have finalized the questions you want to ask, think about the best time to ask these questions of your target audience. If you are asking for feedback on a recent event, for instance, you may have to follow up quickly while the event is still fresh in your target audience’s minds. However, if your survey is not time–sensitive, you can consider sending single–question polls on a regular basis.
An awesome patient experience and excellent service begin with getting to know who your target audience are and what they want from your practice. In order to get that done, you have to gather patient information, and surveys are just a means to achieve that. When reaching out to collect patient information, it is important to get it right from the beginning. The number and types of questions you ask will play an integral role in determining the success of your survey.
There are right questions, and there are wrong questions. Your goal should be to ask the right questions because the wrong questions can get you completely unfitting responses.
If you take the time to write appropriate questions, you will be on your way to getting valuable patient information that can help you drive your practice in the right direction.
Performing a Security Risk Assessment Offers Value Beyond Compliance
The following article is by Art Gross, from HIPAA Secure Now!, the Society’s endorsed HIPAA compliance membership benefit.
As the digital ecosystem continues to thrive and advance, so too must the regulations and practices for safely caring for sensitive data. That is especially true for the healthcare industry, which continues to be a prime target for cybercriminals.
Healthcare practices need to appropriately safeguard electronic protected health information in compliance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Meeting HIPAA requirements and combating cybercrime are not the only battles healthcare organizations face when it comes to protecting their patients. The industry is incredibly susceptible to insider threats, which can cause large, damaging data breaches for organizations.
So, what can healthcare practices do to ensure they’re protecting electronic protected health information (ePHI) and thus, protecting the patients they care for? Start with a Security Risk Assessment.
What is a Security Risk Assessment (SRA)?
Also referred to as a Risk Assessment, or Risk Analysis, an SRA looks at an organization’s administrative, physical, and technical safeguards that are in place to identify security gaps that would pose a potential risk to patient data.
A thorough Risk Assessment will inventory all ePHI repositories, in other words, it will assess and document anywhere the organization may be accessing or storing ePHI. The SRA should also identify threats to those repositories and the current security measures in place to protect the patient data anywhere it is accessed or stored. The SRA should also account for the likelihood of an event (security incident) to occur, and the impact that a security incident (or threat) would have on your organization. A VERY important piece of a thorough Risk Assessment is ensuring that it contains remediation measures needed to lower your organization’s level of risk.
By performing an SRA and detecting risks in the assessment, organizations have a chance to remediate those risks, hopefully before they result in a data breach.
The Department of Health and Human Services notes that the requirement for healthcare organizations to perform a Risk Assessment is pertinent to ensuring the “confidentiality, integrity, and availability of electronic protected health information.”
More Than HIPAA Compliance
It is no secret that performing a Risk Assessment is an important piece in meeting HIPAA requirements. The Office for Civil Rights (OCR) continues to crack down and hand out fines for not complying with HIPAA. In fact, 2018 alone saw over $25 million in HIPAA fines handed out to providers, a reminder that practices should not take this requirement lightly.
Aside from addressing HIPAA requirements, a Risk Assessment can be used to point out vulnerabilities that don’t fall under compliance, but that may lead to a data breach. As cybercriminals become more sophisticated and continue to find new ways to exploit healthcare practices, the industry is reminded that becoming HIPAA compliant alone is not enough to protect them.
If you are interested in learning more about what HIPAA Secure NOW! can do to protect your practice, contact Jonathan Krasner at This email address is being protected from spambots. You need JavaScript enabled to view it.
Protect Your Document Security
The following is from the Society’s endorsed member service, Storage Quarters.
Maintaining an office is never easy. There are a lot of things to keep track of, from day–to–day operations to personnel and tax issues. All of the things that go into running a business or an organization tend to generate a lot of documents. Some of those documents need to be maintained for legal purposes like tax law compliance. And sometimes documents need to be maintained privately, and confidentially.
One category of information that has strong protections against being made public involves health records. And the law that protects the confidentiality of patient health records is the Health Insurance Portability and Accountability Act (HIPAA). At Storage Quarters, many of our document services customers have a major obligation to comply with HIPAA. One of our most popular services is document scanning. And if you handle a lot of documents, you want to make certain your scanned documents are HIPAA compliant. If you are looking for document management services and you want to make sure your scanned documents remain secure and HIPPA compliant, Storage Quarters can help. We don't outsource your document scanning. everything will be done in–house by our staff, which has been trained in HIPPA compliance. They have also passed a background check.
Storage Quarters also provides important document security measures. We’ll encrypt your electronic documents. We’ll set up firewalls and strong disaster recovery programs. Storage Quarters can help you go paperless without compromising document security. Contact us today. This email address is being protected from spambots. You need JavaScript enabled to view it. (516) 794–7300.
New York Maternal Mortality Spikes, Part of Nationwide Issue
The following is by Darrell Ranum, JD, CPHRM, Vice President, Department of Patient Safety, The Doctors Company. The Doctors Company is the Society’s endorsed medical liaiblity insurance company.
According to a report to the New York State Department of Health from the American College of Obstetricians and Gynecologists (ACOG), over the past decade, the state has seen a major increase in maternal mortality.
In 2016, New York ranked 30th in maternal deaths out of 50 states — up from 46th in 2010. The leading causes of maternal death include: embolism, hemorrhage, infection, cardiac disorders, and hypertension. Out of more than 40 maternity hospitals in New York state, less than half of mothers experiencing dangerously high blood pressure got proper treatment, the records show. At some of those hospitals, less than 15 percent of mothers in peril got recommended treatments.Concern over the nation’s rising rate of maternal injury and death has prompted The Doctors Company to review closed claims to identify potential sources of patient injury and provide tools for enhancing safety in ob/gyn, known to be a high-risk specialty. The Doctors Company studied the 490 obstetric-related claims of the 11,289 total claims and suits it closed and coded between 2013 and 2017. Maternal injury accounted for 94 or 19.2 percent of the obstetric claims. The remainder were neonatal injuries. (For more on neonatal injuries, see The Doctors Company’s Obstetrics Closed Claims Study.)
Though they make up just less than a fifth of obstetric claims, maternal injury claims were important to study because about 700 women die from complications related to childbirth in the U.S. each year, according to data from the Centers for Disease Control and Prevention.
Maternal deaths also occur more often in the U.S. than in many other developed countries — a rate of 26.4 per 100,000 live births. The rate is 9 per 100,000 in Germany, 8.8 in the United Kingdom, 7.8 in France, 7.3 in Canada, and 6.4 in Japan. Of great concern, in New York, black women are 3.4 times more likely to die during childbirth than white women.
The Doctors Company’s research showed that 38 percent of maternal injury claims resulted in settlements or judgments — much greater than the average number of paid claims for other physician specialties like general surgery (28 percent), internal medicine (27 percent), and gynecology (31 percent).
The Doctors Company found that two of the most common diagnoses resulting in claims were postpartum hemorrhage, accounting for 15 percent of maternal injury claims, and preeclampsia/eclampsia, making up 9 percent. The rest of the maternal injury claims included these diagnoses:
- Disruption of the perineal wound or complication of a surgical wound: 9 percent
- Placenta previa, placental separation, antepartum hemorrhage: 7 percent
- Tubal pregnancy, ectopic pregnancy: 6 percent
- Maternal cardiovascular disease, cardiovascular disorder, puerperium and postpartum cardiomyopathy: 6 percent
- Spontaneous abortion (no complication and with infection) and incomplete abortion with infection: 5 percent
- Intrauterine death: 5 percent
- Trauma to pelvic organs: 5 percent
- Amniotic fluid embolism: 4 percent
- Perineal laceration: 3 percent
- Infection of the amniotic cavity: 2 percent
- Rupture of the uterus during labor: 2 percent
- Miscellaneous complications: 2 percent
In its closed claims study, The Doctors Company focused on postpartum hemorrhage and preeclampsia/eclampsia because of the high percentage of these claims that resulted in serious injury or death.
Postpartum Hemorrhage Closed Claims
In claims with a final diagnosis of postpartum hemorrhage, injuries included:
- Death: 40 percent
- Organ loss — uterus: 40 percent
- The need for surgery: 27 percent
- Multi–system failure: 13 percent
Since operative deliveries can include vaginal deliveries with the use of forceps or vacuum extraction, as well as cesarean sections, patients may assume that those techniques caused or contributed to the hemorrhage, when in many cases that is not so. So, the allegations in a liability case are not always helpful in understanding what happened.
Therefore, The Doctors Company uses physician reviewers to help it understand the factors that lead to patient injury. In the hemorrhage claims, these experts found that three out of every four claims with a technical performance factor (53 percent) were due to complications and not due to negligence. Only a quarter of the claims with this factor were due to substandard care. Selection and management of therapy was a factor in 47 percent of maternal injury claims. (More than one factor can lead to an injury.) This often refers to a delay in recognizing a problem and taking the necessary steps to correct it.
The cause of a hemorrhage is not always known, but if there is negligence it is most likely to involve a delay in recognition and intervention. Additional factors contributing to patient injury from hemorrhage include conditions affecting the caregiver, such as distractions, multitasking, and interruptions. Those were a factor in 20 percent of the claims.
Staff issues, such as those involving physician coverage, were a factor in 13 percent of injuries.
Postpartum Hemorrhage Case Studies
Consider these examples in which postpartum hemorrhage might have been addressed more effectively:
- Case Study 1
The patient presented to labor and delivery when her water broke. The baby was delivered by cesarean section. The uterus was bleeding, so areas were cauterized, and the incision was closed.
The patient continued to bleed with a boggy uterus. Nurses performed uterine massage, administered Methergine, and applied pressure dressing. The patient became hypotensive and tachycardic. The patient was given several units of blood.
Six hours after delivery, a balloon was inserted for tamponade. Bleeding continued, however, and the patient expired 15 hours later.
Most experts agreed that the response to this crisis was insufficient. The amount of blood loss was not measured. By the time the extent of the crisis was recognized, the patient was seriously ill, and the interventions were too late.
- Case Study 2
The patient was found to have a low–lying placenta, anterior, which increased the risk of accreta. The obstetrician discussed with the patient the possibility of hemorrhage that could occur at delivery and result in a hysterectomy.
The patient underwent a cesarean section. The uterus was normal in appearance and the placenta was removed manually. The patient did not bleed as expected.
The patient had a normal recovery and was discharged on post–op day three. There were no signs of vaginal bleeding. The patient attended her post–op appointment two weeks following her discharge from the hospital.
About three weeks postpartum, the patient presented to the emergency department with complaints of active vaginal bleeding. Attempts were made to examine the patient, but she was bleeding profusely. She underwent an emergency hysterectomy, and did recover.
Experts expressed differing opinions. Plaintiff experts claimed that the obstetrician failed to remove all the placenta from the uterus, causing a postpartum hemorrhage. Defense experts disagreed, stating that products of conception would have caused cramping and bleeding following delivery. Their successful argument described a rare condition called subinvolution of the placental site as the cause of the bleeding.
Preeclampsia and Eclampsia Closed Claims
With preeclampsia and eclampsia, The Doctors Company’s data underscore the importance of closely monitoring a patient's blood pressure.
In closed claims with a final diagnosis of preeclampsia or eclampsia, the injuries included:
- The condition becoming worse: 78 percent
- Death: 56 percent
- Hemorrhage (brain): 33 percent
- Cognitive dysfunction: 22 percent
Patient assessment issues, such as failure to establish a differential diagnosis or to appreciate and reconcile relevant signs, symptoms, and test results, were factors that led to injury in 67 percent of these closed claims. Patients frequently will present with a headache that is often an indicator of high blood pressure that should be treated expeditiously. The longer the delay, the more likely the patient will suffer a stroke or other injury from the excessive pressure.
However, a patient may report headaches to a primary care or emergency physician rather than her obstetrician, not realizing the connection and possible threat to the pregnancy. Ideally, the treating physician will report this concern to the obstetrician, but in some cases the headache is treated but not the high blood pressure.
Communication among providers was a contributing factor in 56 percent of the cases. This often involves failure in communication between nurses and physicians, which can take several different forms. A nurse may take a patient's blood pressure, note that it is high, but get called away and distracted before reporting this critical value to the physician. Or the nurse may call the physician with that information, but the doctor does not communicate treatment instructions to the nurse or another physician who is present.
Off–hours conditions for providers working on weekends and holidays were found to be contributing factors in 33 percent of the closed claims. Staffing may be limited during off–hours, and if there is not an adequate policy and process for calling in additional help, patients with elevated blood pressure or preeclampsia may go longer than normal without being treated. Selection and management of therapy also was found to be a factor in 33 percent of cases including management of pregnancy and failure to order medication.
Preeclampsia and Eclampsia Case Studies
- Case Study 1
Over the course of two months, a pregnant patient had increasingly elevated blood pressures and increasing amounts of protein in her urine. She also developed headache and was prescribed bed rest.
The patient’s symptoms did not improve, so an obstetrician recommended induction. The nurse midwife communicated the recommendation to the patient without explaining the clinical rationale. The patient declined. The nurse midwife did not communicate this information to the obstetrician. The following day, the extremely elevated results of the patient’s 24–hour urine protein were received.
A short time later, the patient presented to the emergency department with severe abdominal pain. Her blood pressure was 197/111. The patient was admitted and taken for a cesarean section.
Following the delivery, the patient’s blood pressure remained elevated. Attempts to reach the physician were unsuccessful. A few hours later the patient vomited. A short time after that she was found unresponsive. A CT scan showed intracranial bleeding. The patient expired later that evening.
Experts opined that the patient should have been delivered earlier due to the protein in her urine. Clinicians were also criticized for not investigating the causes of headache. The risks of delaying delivery were not explained to the patient. Experts expressed concerns about the patient’s postpartum management and the failure of nurses to have a physician evaluate the patient when her pressures remained so high after delivery.
- Case Study 2
The patient had a cesarean section and two days later was discharged with a normal blood pressure reading. Eight days later, she presented to the emergency department with a severe headache and elevated blood pressure (172/104). She was treated with a pain reliever and discharged when the pain decreased.
Four days later, the patient met with her obstetrician complaining of continuing headache. Her blood pressure was still elevated. Her physician ordered medications for elevated blood pressure and headache. Lab results showed elevated uric acid and normal liver enzymes. No urine protein was ordered.
After another four days, the patient presented to the emergency department complaining of severe headache and slurred speech. Her blood pressure remained elevated (183/97). A CT scan showed hypodense areas in her cerebellum. She was diagnosed with postpartum eclampsia and vasospasm.
The patient was admitted to the ICU, where her condition continued to deteriorate. She slipped into a coma and expired.
Experts differed on the patient’s diagnosis and a recommended treatment modality. Even with differing opinions, it was clear that multiple clinicians failed to take definitive action to reduce the patient’s blood pressure and prevent the cerebrovascular accident.
Discussion
Accurate blood loss assessment: In some of the hemorrhage cases, patients were observed having continued bleeding after delivery, but the measures taken were not adequate. It was clear that in many cases the nurses and physicians providing care did not recognize the extent of the bleeding soon enough. A contributing factor was that blood was absorbed in blankets and towels so that it was difficult to quantify unless those items were weighed before and after blood absorption. It is only from accurately assessing the blood loss that clinicians can recognize the problem early and intervene in the most effective manner. Routinely weighing blood–absorbent materials is the standard of care, yet many institutions do not follow this practice, and instead wait until clinicians perceive excessive blood loss.
Communication: Timely communication among clinicians is essential for early interventions. Closed–loop communication confirms that both parties share understanding of the situation, which increases the chances of an adequate response to patients’ crises. Communication between clinicians and patients and their families is also crucial. Some maternal injuries are unavoidable with the best of care, and regardless of the cause, physicians and hospitals should communicate openly with patients who suffer unexpected outcomes. Honesty is important, and that includes explaining the results of internal investigations. Even when the care provided was appropriate, physicians and hospitals must take the time to help patients understand what happened. When negligence has caused patient harm, physicians and healthcare organizations are usually willing to negotiate settlements and provide compensation.
Risk Mitigation Strategies
To prevent maternal injury and death, The Doctors Company recommends that healthcare providers and hospitals consider the following steps:
- Adopt best practices from the American Congress of Obstetricians and Gynecologists (ACOG) patient safety bundles.
- Institute proper triage and screening tools so early warning signs are not missed.
- Create a culture of patient safety.
- Practice simulation to be ready for unexpected, rare events.
Additionally, a successful program to reduce maternal mortality, first tried in California, could be adopted in other states. The California Maternal Quality Care Collaborative, an organization of more than 200 hospitals, helped to reduce California’s maternal mortality by 55 percent between 2006 and 2013, while the national mortality rate continued to rise. The Collaborative has accomplished this by providing hospitals with access to near real-time benchmarking data through its online Maternal Data Center. The Center links state birth certificate data with each hospital’s patient discharge data to generate perinatal performance metrics and quality improvement insights.
.
Maternal morbidity was reduced by 20.8 percent between 2014 and 2016 among the 126 hospitals participating in projects to reduce maternal hemorrhage and preeclampsia. Initiatives like this should be considered in every state to improve the quality of care to pregnant women. Doing so enhances the chances of safe deliveries, healthy infants, and healthy mothers who retain their ability provide the care that these families need.
Updated Workers’ Comp Schedule Auto No–Fault Delayed
The New York State Department of Financial Services has decided to delay implementation of the recently updated Workers’ Compensation Medical Fee Schedule until October 1, 2020 for the Auto No-Fault Program.
Therefore, you will need to keep the Workers’ Compensation Fee Schedule that was effective on June 1, 2012 for billing claims for the treatment of persons injured as the result of auto accidents.
Public comment can be sent to This email address is being protected from spambots. You need JavaScript enabled to view it. before April 22, 2019.
CMS Issues Quality Payment Program: 2019 Resources
Cross-Cutting Quality Measures: List of cross–cutting Quality measures that are broadly applicable to all clinicians regardless of their specialty
Quality Measure Benchmarks: Lists and explains benchmarks used to assess performance in the Quality performance category
MIPS: Summary of Cost Measures: Summary of cost measures
Improvement Activities Inventory: List of the improvement activities and descriptions
MIPS Participation and Eligibility Fact Sheet: Overview of the eligibility criteria
Cost Performance Category Fact Sheet: Includes details on the episode–based measures
Free CME Program on Adolescent Sexual Health
The NYC STD Prevention Training Center at Columbia University is offering a one–day Adolescent Sexual Health Symposium for CLINICAL providers on March 26, 2019. Physicians, physician assistants, nurses, and nurse practitioners are welcome to attend. Continuing Education will be available. Please register at: https://courses.nnptc.org/class_information.html?id=2474. Your registration is not complete until you receive a CONFIRMATION EMAIL from This email address is being protected from spambots. You need JavaScript enabled to view it..
As a member, you are entitled to attend Society meetings and functions. Keep track of what
is going on by checking this listing in every issue of MM “NEWS.” Members are invited to
attend any of these sessions; however, we suggest that you call (212) 684–4670 to confirm
meeting date and time.
— Thursday, March 21, 2019, 6:30 p.m. to 8:30 p.m. Physician Well-Being: Threats, Consequences and Solutions, with Jonathan Ripp, MD, MPH, Conference Room A117, Mass Mutual, 277 Park Avenue, New York, NY 10166, (between 47th and 48th Streets). Light food & beverages provided. No charge but advanced registration required. Space is limited. Register with Lisa Joseph, (212) 684–4698 or This email address is being protected from spambots. You need JavaScript enabled to view it.
— Thursday, April 18, 2019, 5:30 p.m. to 8:00 p.m. An Evening of Risk Management CME: “Personal Electronic Device Distraction and the Threat to Patient Safety” “Electronic Health Record: Ten Years and Still Risky” at the Midpoint Bistro, 40 West 45 Street, New York NY 10036 (between Fifth and Sixth) with the New York County Medical Society and the Doctors Company. No charge, but pre–registration required; light supper; 2.5 CME Category I. Register with Lisa Joseph, (212) 684–4698 or This email address is being protected from spambots. You need JavaScript enabled to view it.
Dues Deductions for 2018 Taxes
Just a reminder that because of change in tax laws, membership dues are still deductible only as long as the member is filing a Schedule C (Profit/Loss from Business or Profession) or it’s flowing through a corporate return. In that case, 30 percent of the Medical Society of the State of New York dues, and ten percent of Society dues are not deductible
Please note, you can no longer treat dues as a miscellaneous itemized deduction.
If you have questions, discuss with your accountant.
How Can You Save When You Bill?
PS2 Practice Management is the endorsed vendor of the New York County Medical Society for medical billing services.
Medical billing can be a challenge for private practitioners. Some of the challenges faced by physicians in private practice include spending lengthy amounts of time on the phone with insurance companies trying to obtain a prior authorization to fighting denials and writing appeals for the same claim over and over. PS2 Practice Management can step in and alleviate this burden on physicians and their practice staff.
How do we do this? PS2 will initiate and manage the prior authorization process for the practice. The PS2 team will contact the insurance company and initiate the prior authorization request. Once the authorization is received, PS2 will communicate this information back to the practice. This saves the physician and staff from having to spend what can often amount to hours on the phone with the insurance companies.
The billing process begins when the practice provides the information to be billed out. The PS2 billing team will enter these charges into the billing system and send the claims out electronically. Should the insurance company require additional information, the PS2 team will reach out to the practice.
Denial management is also handled by the PS2 team. For a private practice, often the practice staff does not have the time to dedicate to denial management which can result in loss of revenue for the practice. Having a dedicated team focus on denial management ensures they are handled in a timely manner and get the attention and focus necessary. PS2 will monitor and report monthly on key metrics that are important to your practice; including days in A/R and collection rates.
PS2 also offers additional specialized services such as coding, contracting and credentialing.
Let the PS2 Practice Management team assist you with all your medical billing needs and give you and your practice staff time to focus on patient care. To learn more, please contact Jennifer Cross at This email address is being protected from spambots. You need JavaScript enabled to view it. or ( 847) 228–3320.
The following 21 candidates for membership have been presented to the Board of Directors of the Society.
Dena M. Abdelshed, MD
Amit Aggarwal, MD
Ariel M. Anderson, MD
Grigory Arutyunyan, MD
Nicolas Bavaro, MD
Steve B. Behrens, MD
Mark Brouillette, MD
Saadia Chaudhary, MD
Chris Clifford, MD
Julie Foont, MD
Michael P. Glick, MD
Oliver Harper, MD
Julie H. Y. Huang, MD
Sravisht Iyer, MD
Lloydine Jacobs, MD
Scott Katzman, MD
Brian Mayrsohn, MD
Carlo J. Milani, MD
Jonathan Overdevest, MD
Douglas Alan Slaughter, MD
Michael S. Virk, MD
Tips for Medical Practice Recruiting Success
Medical Staffing is a specialized task that helps to build the foundation of a medical practice. Finding the right people who are not only committed, but also qualified, can be daunting at times. In recruiting, here at Winston Medical Staffing, we sometimes come across roadblocks that make finding the right candidates hard, even with sourcing and referral programs. There are methods that you can adopt to help keep your pipeline running strong. Streamlining your approach using some tips from Winston Medical that can help make the recruitment process run more smoothly. This is especially true for the healthcare industry, as there are constant changes, cutbacks, and frequent updates that affect your candidates.
Understanding the needs of the medical professional: Whether the position you are seeking to fill is a nurse, medical assistant or medical secretary — you need to know what characteristics the candidates are looking for in potential employers. Knowing about the skill sets is the best way to begin to search for the appropriate candidates. Recruiting at its core is more than simply finding people who have the skills; it is also about finding people who have the drive, passion, and fit for the practice. Connect with the candidate by trying to get an insight into their current role’s needs and challenges. This will give you much needed insight in staffing this role.
Positioning your practice: When medical professionals are searching for their next opportunity, they are not just looking for another job that will be like their last. They are looking for a whole new experience in itself. In a way, these candidates are “shopping” for their next employer. When creating your job posting, you need to have a catchy company profile to get the candidate excited about what could potentially be around the corner. Talk about benefits, give insight into the work culture and the value that the organization places on its employees. Give a glass door look into the practice that allows the candidate to brainstorm about how the organization will fit into their lifestyle.
Get in touch with professional associations: Connecting with professional bodies in the healthcare industry can be an excellent way to connect with potential candidates. Typically, when candidates join a professional body, it is because they want to get an advance on their career. They will utilize the resources that the association offers them to network, work towards designations, and more. Getting your posting on their job boards or going as a guest to networking events can be a great way to see and hear firsthand what employees are really looking for. By being a member of the New York County Medical Society, you have already taken that important first step.
Have a current temporary or direct hire staffing need for your practice? If so, talk to a staffing firm with a focus on your industry. In this case, Winston Medical Staffing, a JCAHO–certified agency with over 50 years in the industry is the New York County Medical Society’s endorsed medical staffing partner and can help you find the best talent for your company's culture, goals, and specific needs. Winston provides temp, temp to direct hire and direct hire placements. We also have a 24–hour service center for last–minute staffing needs. For more information, feel free to contact Ivy Kramer, MSW, CSW your designated account representative at (212) 687–4667 or email at This email address is being protected from spambots. You need JavaScript enabled to view it.
DocbookMD, a HIPAA–secure communication solution for physicians, is offered as a free benefit through the New York County Medical Society. . Designed by physicians, for physicians using smartphones and tablets, it allows you to send HIPAA–compliant messages bundled with photos of x-rays, EKGs, wounds, and more. Just as if you were sending a text.
For more information please visit docbookmd.com or contact DocbookMD at (888) 204–0053.
In 2016 the American Medical Association (AMA) and a number of other health–related organizations partnered to establish Xcertia, with the goal of developing guidelines for safe and effective digital health apps that will facilitate virtual care, including remote patient monitoring for chronic diseases. This is an emerging set of technologies, which is largely unregulated. Many solutions are not evidence–based and have not demonstrated that they are safe and effective tools for use as part of a patient’s treatment plan.
Xcertia has now released a complete set of guidelines covering the privacy, security, operability, usability and clinical content of mHealth solutions: https://xcertia.org/news-announcements/. The guidelines are now available for public comment until May 15, 2019 at: https://www.xcertia.org/the-guidelines/. Xcertia will rely on these public comments to create a final version of the guidelines.
Xcertia welcomes your comments and encourages you to join with us in recommending the guidelines to developers and physicians as a resource when considering mHealth solutions for their practice and to recommend to their patients.
For questions, comments or if you wish to join this effort, please contact Michael L. Hodgkins, MD, VP & CMIO, AMA at This email address is being protected from spambots. You need JavaScript enabled to view it..
Citiwaste is now an exclusive provider of medical waste management services offering deep discounts to New York County Medical Society members. Whether sharps, red–bag, chemo, pathology, hazardous, or pharmaceutical waste, Citiwaste will work with you to classify and segregate waste streams for best pricing.
In addition, Citiwaste will determine the appropriate service frequency and deliver the supplies you need to package wastes. Guaranteed savings with no fuel, stop, energy, or environmental fees. Medical waste manifests available online 24/7 at no charge. One provider for all your medical, hazardous, and pharmaceutical waste.
Protection for your business with complete regulatory compliance. Call David at (718) 372-3887 to learn more about how Citiwaste can save you money.
The U.S. Air Force Health Professions Office handles applications for the Office of the Surgeon General’s following programs:
1. Medical Corps Health Professions Scholarships Program
(Up to 100% Tuition & Fees Scholarship for 4 years, with $2,330/month Stipend, $20K Sign-up bonus, and materials reimbursement quarterly)
a. Undergraduates and graduates applying to medical school
b. Current medical school students
c. Students already enrolled in early assurance programs at the undergrad or graduate levels
2. Medical Corps Health Professions Financial Assistance Program
(Earn up to an additional $73K per PGY on top of what their residency program is already paying)
a. Final year medical school students playing in the match cycle
b. Final year medical school students already matched
c. Current Residents
d. Current Fellows
The office also manages the U.S. Air Force Medical Service and associated organizations’ manpower:
3. Direct Accessions of BE/BC Physicians
(Initial Sign–on bonuses from $250–400K depending on specialty + competitive pay and unmatched benefits)
a. Final year residents and fellows
b. Practicing Physicians seeking a change, challenge, or privilege to serve
c. Any ‘a’ or ‘b’ candidate wanting to gain additional training, licensing, and experience as an Aerospace Medicine Doctor (a.k.a. Flight Surgery or Flight Medicine)
d. A pathway to highly specialized and elite physician programs and teams like Special Operations Surgical Teams (SOST), Critical Care Assessment Teams (CCAT), Ground Surgical Teams (GST), Center for Sustainment of Trauma and Readiness Skills (CSTARS) and many, many, more growth and career broadening pathways.
For information contact Sean C. Triglia, SSgt, USAF, U.S. Air Force Health Professions Office
Medical Corps Physician Officer Program Manager, Board Certified Full–time Accessions
Office: (212) 233–4560 x 202, This email address is being protected from spambots. You need JavaScript enabled to view it.
Jay Gold Barnett, MD, died November 13, 2018. Doctor Barnett received his MD degree from State University of New York, Syracuse in 1964.
Leon Lefer, MD, died February 2019. Doctor Lefer received his MD degree from University of Lausanne Faculty of Medicine in 1952.
Norman Orentreich, MD, died January 2019. Doctor Orentreich received his MD degree from New York University School of Medicine in 1948.
Elisabeth L. Macrae, MD, died May 3, 2018. Doctor Macrae received her MD degree from Medical College of Pennsylvania in 1968.






